Healthy communities spotlight
In the Waikato region, 41 percent of the population lives in rural areas. However, the rural health workforce is aging, with many nearing retirement.
On this page

Braemar
In the Waikato region, 41 percent of the population lives in rural areas. However, the rural health workforce is aging, with many nearing retirement.
There is a stark need for healthcare services, but the current medical training system contributes to inequity. Few qualified individuals choose to work in rural areas, and the Auckland School of Medicine only offers limited placement options, with no placements from the Ota go School of Medicine in the South Island.
The lack of accessible health services contributes to disparities in life expectancy and illness experiences between rural Māori, rural populations, and non-rural populations.[3]
Key statistics include:
- Māori males have a life expectancy that is 8 years shorter than Pākehā males, while Māori females have a life expectancy that is 7 years shorter.
- Pacific females and males have a life expectancy that is 6 years shorter than Pākehā[4]
The demand for health services is expected to remain high in rural Waikato, particularly in the most deprived areas such as Ngatea, Kerepehi, South Paeroa (Hauraki DC), and Tokoroa (South Waikato DC). However, the population size is not projected to increase significantly.
While delivering rural services remains a challenge, it's worth noting that urban Hamilton, despite being one of the more deprived areas, will continue to drive greater demand for health care services. Additionally, the demand for healthcare services in Hamilton is expected to increase by 30.3 percent or 53,600 people by 2048. The city's diversity will also grow, with a decrease in the Pākehā population and an increase in Māori, Pacific, and Asian populations.
Ngāruawāhia and Huntly, which also experience higher levels of deprivation, are projected to undergo significant population growth by 2048. The Waikato District, including Huntly and Ngāruawāhia, will see an increase of 31,600 people or 36.7 percent, which is equivalent to adding another Thames-Coromandel district. Overall, there is a pressing need for enhanced healthcare services in both rural and urban areas of the Waikato region to address disparities and meet the growing demand for care.
Currently, the Waikato region heavily relies on a migrant workforce, particularly in the healthcare sector. For instance, international qualified nurses (IQN), make up 11.7 percent of the workforce, ranking the region third in Aotearoa New Zealand after Auckland and Canterbury.
Within the wider healthcare workforce, the residential care services sector (mainly aged residential care) has the highest proportion (25.58 percent) of workers on a migrant visa, slightly higher than the national average of 23.5 percent. Most of these workers are recent residents who entered under the skilled migrant category (33.1 percent).
Hospitals in the Waikato have 13.8 percent of their workforce on a migrant visa, again slightly higher than the national average of 11.6 percent. Of these, 56 percent are recent residents under the skilled migrant category. Medical and other care services have only 7.1 percent of their workforce on a migrant visa, and like the previous categories, most are recent residents who entered under the skilled migrant category.
The Aotearoa New Zealand trained medical workforce in the Waikato lacks diversity. Only 8.4 percent of Aotearoa New Zealand qualified nurses who identify as Māori work in the region, while Māori make up 23.9 percent of the population. Similarly, only 6.7 percent of Aotearoa
New Zealand qualified nurses who identify as Pacific work in the Waikato, despite Pacific people comprising 4.5 percent of the population.
The Health and Disability System Review Final Report in 2020[5] emphasised the importance of having a diverse and representative healthcare workforce to deliver equitable health services. However, Māori are under-represented in medical, nursing, midwifery, allied health, and scientific roles that offer higher pay. The lack of diversity is visually depicted below.
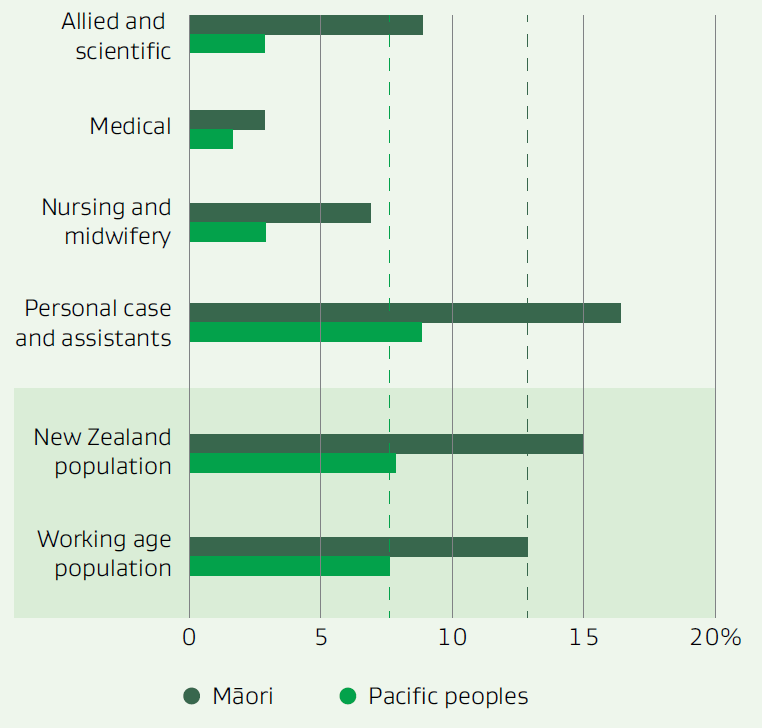
Data for image
In addition to the lack of diversity, the Waikato region is not training healthcare professionals at the required levels to meet future demand. Based on the average completion rate over the past three years and the projected job openings in the sector until 2028, there will be an insufficient number of trained individuals at levels 1 to 3 (Kaiāwhina/Health Care Assistant roles) to fill the job openings. Moreover, there will also be an insufficient number of individuals trained at degree level 7 and above to fill expected job vacancies. These roles include Registered Nurses, Medical Practitioners, and allied health professionals such as Sonographers, Pharmacists and Physiotherapists. The top 10 occupations across the health sector in the region are shown in Figure 2.
Figure 2. Top 10 occupations by job openings
- Registered Nurse (Medical)
- Nurse Manager
- General Medical Practitioner
- Resident Medical Officer
- Physiotherapist
- Registered Nurse (Mental Health)
- Occupational Therapist
- Registered Nurse (Community Health)
- Nurse Educator
- Nurse Practitioner
The Waikato Region requires:
- 2,000 nurses to fill job openings over the next 5 years
- 463 medical practitioners with 168 GPs (35 percent of the total forecast and this is where the greatest need is)
- 7,273 Kaiāwhina/HCAs to fill job openings in the next 5 years
Recommendations
- Train and/or recruit more rurally based health professionals to meet demand
- Leverage Māori and Pacific to train in professional clinical roles like nursing, medical and allied health
- Upskill the many Māori/Pacific in Kaiāwhina and health care assistant roles, into professional medical roles
- Encourage and mentor secondary students into health professions with a focus on Māori and Pacific students
- Consider the role of migrant workforce and ensure that they are welcomed and utilised to their skills levels and encourage then to upskill
- Provide input into the development of the Rural Health Strategy being developed by the Ministry of Health
- Consider the recommendations made in The Rural Health Strategy due to be published in July 2023
Actions
Advocate to remove barriers and fast-tracking in the health sector with a focus on local and migrant training:
- Promote Māori and Pacific students to take health, science and maths-based subjects at secondary school
- Support/advocate for initiatives that attract/ retain Māori and Pacific students into careers and relevant internships within health
- Support Māori into mentoring and leadership training
Promote for employer skill needs to be met in the health sector, especially in Kaiāwhina roles:
- Identify learn-as-you-earn training and development opportunities to upskill Kaiāwhina noting the needs to be flexible, low-cost and close to home
Footnotes
[3] Sapere, 'Rural lnterprofessional health Schools' March 2020
[4] Te Whatu Ora Waikato
[5] New Zealand Health and Disability System Review I Final Report March 2020

